What is alpha-1 antitrypsin deficiency?
Alpha-1 antitrypsin deficiencyAlso known as AATD. A genetic disorder with multiple manifestations, including lung dysfunction and progressive liver disease. (AATDAlso known as AATD. A genetic disorder with multiple manifestations, including lung dysfunction and progressive liver disease.) is an inherited condition that increases the risk of liver and lung disease. AATD is caused by mutations (i.e., changes) in the SERPINA1The gene which encodes the alpha-1 antitrypsin (A1AT) protein, commonly leading to lung dysfunction and liver disease. gene. This gene provides instructions for making alpha-1 antitrypsin (AAT). AAT is a protein predominately made in the liver that helps maintain healthy lungs. If the SERPINA1 gene is mutated, it will make an abnormal AAT protein.
When a person has alpha-1 antitrypsin deficiency, their AAT protein levels in the blood and lungs are very low, because the abnormal protein accumulates in the liver. The shortage of protein in the blood and lungs places the lungs at risk for emphysema, a type of chronic obstructive pulmonary disease (COPD). Due to the abnormal protein accumulation, people with AATD also are at risk for progressive liver disease.
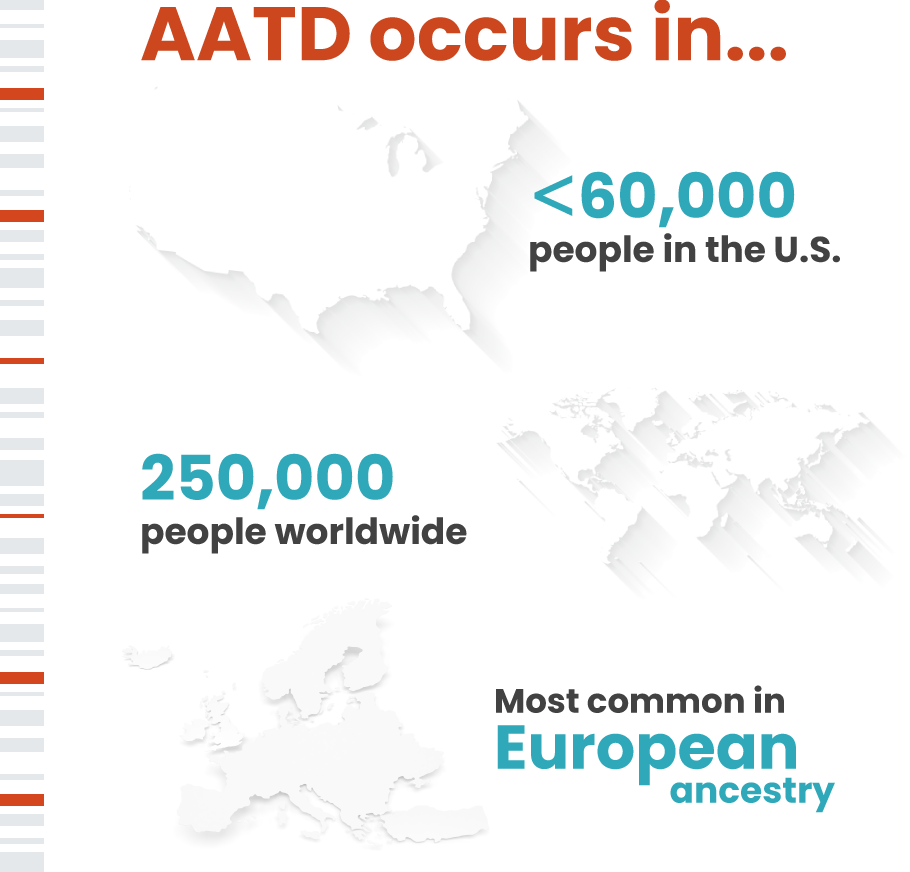
AATD occurs in less than 60,000 people in the U.S. and around 250,000 worldwide. It is most common in those with European ancestry.
What are the symptoms associated with alpha-1 antitrypsin deficiency?
Symptoms of lung disease associated with AATD may include

Shortness of breath, reduced ability to exercise and wheezing
Frequent respiratory infections

Fatigue

Rapid heartbeat

Weight loss
Yellowing of the skin and whites of the eyes (jaundice)*
Swollen belly, feet or legs from fluid retention*
* Late stage AATD-related liver disease symptoms experienced by some adults and about 10% of children with AATD
How is alpha-1 antitrypsin deficiency diagnosed?
To confirm an AATD diagnosis, a clinician may order several tests, including:
- blood tests to measure AAT protein levels and types
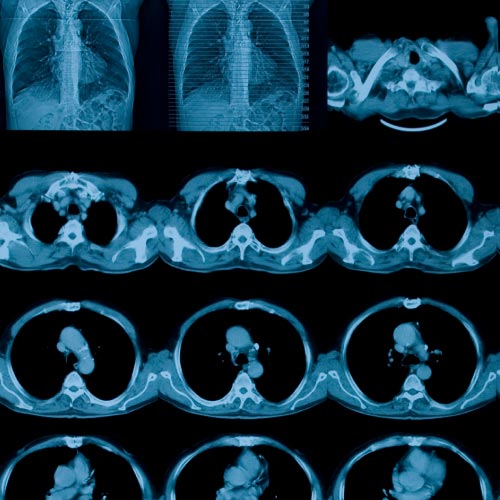
- imaging tests to determine if there is any damage to the lungs or liver
- genetic testing to identify abnormal AATD genes

How is alpha-1 antitrypsin deficiency treated?
Currently, there is no cure for AATD, and some people require lung or liver transplant.
Treatment is focused on managing symptoms and preventing further damage. For the lungs, this includes avoiding cigarette smoking, as well as other environmental exposures such as pollutants. For the liver, maintaining a healthy weight, avoiding excessive alcohol intake and vaccination against viral hepatitis may be helpful.
In special circumstances, replacement (augmentation) therapy is used to raise the amount of AAT protein in the blood and may slow lung damage. Medications, such as steroids and bronchodilators, can open the airways to help with breathing.


